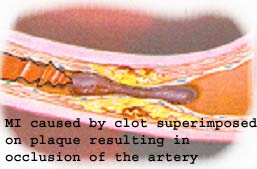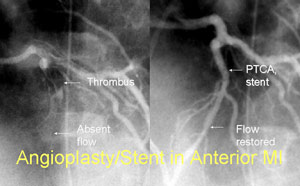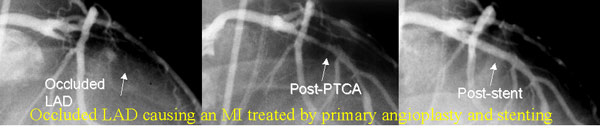
Acute Myocardial infarction (heart attack MI) results from occlusion of one of the coronary arteries of the heart by thrombus (blood clot) often superimposed on a ruptured plaque (atherosclerosis, blockage). It often starts with uncomfortable pressure, fullness, squeezing or pain in the center of the chest lasting more than a few minutes; Pain may spread to the shoulders, neck or arms. Chest discomfort may be associated with lightheadedness, fainting, sweating, nausea or shortness of breath, unexplained anxiety, weakness or fatigue, Palpitations, cold sweat or paleness). Immediate Medical Attention and prompt treatment with Aspirin, blood thinners, and either a clot busting (dissolving medicine) such as tPA, rPA, streptokinase, or immediate cardiac catheterization with primary angioplasty of the occluded artery to abort the heart attack. When available promptly (such as BIDMC), primary angioplasty improves the outcome of patients with heart attacks. Other medications used are beta blockers, nitroglycerine, and ACEinhibitors, statins, and platelet inhibitors. Prompt treatment is essential to minimize the extent of damage to the heart.